#POCUS for DVT in the ICU: Can it be Done?
Anton Helman (@EMCases) from EM Cases brought up a recent article on Twitter regarding DVT POCUS performed by internal medicine residents in the ICU. The results were…disappointing…
But does this spell the end for DVT EDE? Let’s peel back the layers of the onion & see. If you would like to read the article yourself, click here for the Pub Med link. The reference is: Caronia J et al. Resident performed two-point compression ultrasound is inadequate for diagnosis of deep venous thrombosis in the critically ill. J Thromb Thrombolysis 2014;37:298-302.
Where?
- ICU in 625-bed Lenox Hill Hospital in NYC
When?
- 9 consecutive months in 2010-11
Who said they need a scan?
- Patients who were suspected clinically by ICU staff of having a DVT
Who did the scan?
- Internal medicine residents on a 2-4 week elective in ICU.
What training?
- 2 hours combined didactic & practical. Unknown: prior training of residents in other types of POCUS
How was the scan done?
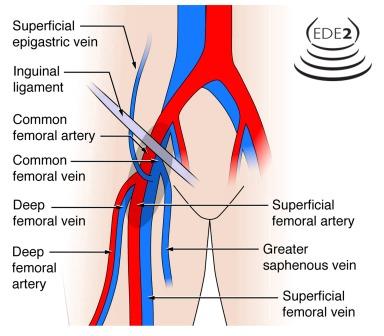
- B-mode compression only of common femoral, saphenofemoral junction, and popliteal. Not done: superficial femoral, calf veins, routine Doppler
Compared to?
- “Comprehensive” Doppler (presumably whole leg?) performed by tech and interpreted by blinded staff rad
The Boxscore:
- 19 residents did 143 scans on 75 patients (i.e. most patients had both legs scanned)
- a mean of ~ 7.5 scans was done by each resident (range: 2-23)
- 21 patients had a DVT (6 common femoral, 9 popliteal, 6 superficial femoral [NOTE: no indication if these were just below the takeoff of the deep femoral or if the DVT was in the mid-thigh])
- 13/21 DVTs were picked up by the residents. 2 popliteal DVTs and all 6 superficial femoral DVTs were missed. This makes for a low sensitivity of 63%.
- elective ultrasound took 14.7 hours to be reported!
- based on the residents estimate, each scan took an average of approximately 5 min to perform [not precisely measured and slower than the Blaivas study where a scan took 2.5 min]
Let’s Discuss…
- We don’t know what training the residents received in basic POCUS prior to the study. If they had none, then it’s unrealistic to expect that they would pick up on how to do a DVT scan in a 2-hour session. Even with a solid base, the DVT scan probably needs somewhere in the neighborhood of 25 training scans (after a course) on real-world patients to become competent.
- The superficial femoral vein was not scanned. In EDE 2, we teach that the first 2-3 cm of this vein should be scanned (see the figure at the bottom of this post). Had this area been scanned, some of these DVTs may not have been missed. Hard to know. There is no indication of where in the superficial femoral that these DVTs were located. We also teach that one should scan the popliteal vein from its most proximal to its most distal extent, even including the first couple cm of calf veins. Is this how the scan was performed in this study? Can’t tell.
- ICU and ED patients are different populations. Isolated mid-thigh DVTs in ED patients are rare. As the authors point out, ICU patients may be at greater risk for developing mid-thigh DVTs. Many of their patients are intubated and sedated for days! Can one scan the whole thigh to look for a DVT throughout the superficial femoral? Sure, and once fully trained in the technique, it would only add a minute to the scan. What eats up time for the tech is burning images for the rad and doing the Doppler assessment, which adds nothing in the vast majority of patients.
The Last Wave
- With more training than was done prior to this study, we strongly suspect that internal medicine residents would be able to competently perform DVT POCUS.
- Although scanning only in the groin and behind the knee may be sufficient in the vast majority of ED patients, this study suggests that it may be necessary to scan the mid thigh in ICU patients.







Agree. Prof Lichtenstein would recommend scan the sites of central lines also,not just lower limb.