Scrotal ultrasound: it’s what’s inside that matters
Editor’s note: Testicular torsion is a scary condition that we can’t afford to miss. It cannot be diagnosed on history and physical alone in almost 50% of cases so ultrasound is crucial to decision-making. POCUS can be extremely helpful in detecting the torted testis but it is important to understand that a partially torted, or recently detorted testis can have blood flow on doppler imaging. The bottom line is that anyone with a negative scan but reasonable pre-test probability of torsion should go on to urological consult, further imaging, or careful observation and follow-up.
When I teach testicular POCUS I recommend that if you see blood flow in the affected testis on power doppler, you should further assess this flow to confirm there is both venous and arterial waveforms. This is done using spectral doppler, which is a little more complicated than power doppler when in comes to the knobology. A partially torted testis can still have arterial flow while lacking venous flow.
Another trick is to image the spermatic cord. Loss of blood flow or a snail-like mass in the cord (aka whirlpool sign) is another great indication for torsion.
Inhomogeneity of the testicular tissue, decreased power doppler flow, or lack of venous wave forms on spectral doppler indicate torsion until proven otherwise and are indications for urgent urological consultation. [Ed.]
Lloyd’s Cases:
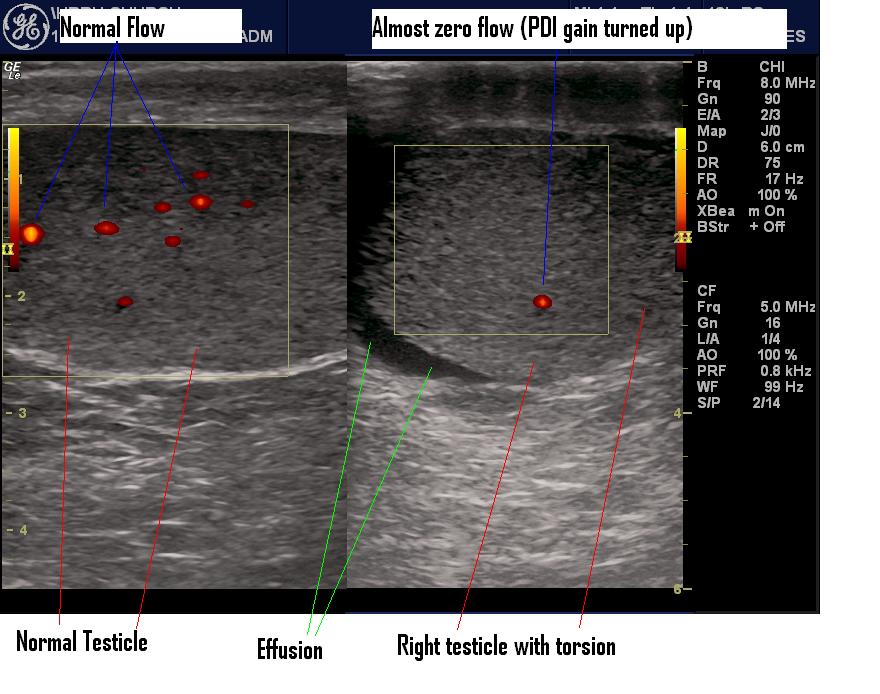
I’ve picked up two testicular torsions recently. It’s actually one of the easier POCUS things to do and is very important and timely. You will have the diagnosis within a minute or two and it’s highly reliable (You always have a control.). The testicles are very easy to image. Just place the linear probe (vascular access or nerve-block presets will do). Center the testicle in the screen-it will have a very homogeneous texture. Look for a scrotal effusion at the bottom of the screen-it’s size will reflect the torsion time. Then turn the PDI (power doppler) on. You can use colour doppler too but I think PDI is easier. Look at the PDI on the painless testicle first. Adjust the PDI gain to get lots of bright spots. Switch sides. If there is torsion, there will be far fewer (almost none) bright spots. I like to get a split screen to get shots of both testicles PDI for comparison and storage.
So if you see much less flow (probably with an effusion) call the urologist before the technologist does the U/S. I get the U/S anyway because hardly anybody believes my POCUS. If you’re not sure get the U/S anyway and proceed as before POCUS.
To get practice, anytime you have a renal colic where the POCOS doesn’t show hydro, check the testicle (male patients only 😀 ).