Do you use M-mode much?
There are two types of EM POCUS users, those that use M-mode all the time and those that rarely use it.
As a POCUS educator I teach M-mode for various applications but admit that I apply it sparingly, often using the “eye-ball” technique for cardiac and pulmonary scans. When it comes to impact on clinical decision making, I find it is usually the more extreme findings easily appreciated on the B-mode image that best guide management. An IVC that completely flattens or barely moves during respiration doesn’t require M-mode to sort out. Everything in-between is taken with a grain of salt.
I know many disagree on the utility of frequent M-mode use. Working in a very busy community ED I try to be as efficient with my scans as possible. Scanning while taking the rest of the history, bringing the machine into the room at first contact, having gel and towels stocked and accessible on the cart, and focusing on those findings that directly guide management and can often be assessed in 60 seconds or less. That is the way I can get a lot of scans done while maintaining excellent patient flow.
Unlike doppler, M-mode is fairly easy to learn and perform. The problem is that it slows things down the moment you start trying to line everything up and do your measurements. It is not unusual for the patient or probe to move requiring re-aligning your M-mode line again.
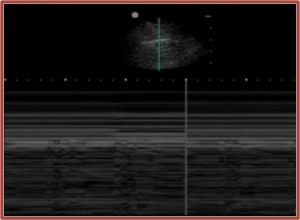
Some swear M-mode helps them with their pulmonary scans. The classic barcode and seashore signs we all love to teach so much. I rarely have trouble appreciating lung slide on B-mode myself, particularly when appropriate ultrasound settings for lung are used, (which I see a lot of clinicians fail to do.)
If you are into carefully assessing RV function in your patients, M-mode can certainly be useful. I just don’t find I do this often compared to the rest of my scanning on any given shift.
I probably use M-mode for fetal heart rate assessment as much as for anything else and it doesn’t change my management much. The slow fetal hearts are usually pretty easy to appreciate.
But wait, maybe we aren’t as good at eyeballing things as we think in the ED. The authors of this paper make their case for using M-mode more often in EM practice.
M-Mode for the EP Ultrasound in EM June 2015
This article suggests we do a better job at assessing LV function and hypertrophic cardiomyopathy using M-mode and EPSS.
EPSS measurement Am J of EM 2014
Other studies suggest novice users applying M-mode achieve results comparable to experienced users, more so than with eyeballing things. So should we be emphasizing M-mode more until neophytes develop their own “ultrasound eye”?
Performance of emergency physicians in point-of-care echocardiography following limited training
Bottom line is that I find M-mode very useful but in a small and select number of patients. I spend more time teaching it than using it. Is it time to embrace the MMM-mode?
I would love to hear your opinions and about your experience regarding M-mode in the emergency department setting.







Hi. In my humble view, a POCUS experienced physician doesn´t need M-mode for decision making in everyday practice. A POCUS non-experienced physician doesn´t need M mode also, since it adds confusion if 2D findings are not clear. In this last case, is preferable, professional, safer and reassuring to make a consultation with an experienced practitioner in place of using M-mode.
Interesting debate. I won’t chime in with detailed comments…just to say to aside from mentioning M-mode in the Thoracic chapter, it otherwise does not appear in EDE 2, except to dissuade participants from using it. If one is so uncertain about the presence or absence of lung sliding, we would rather folks call their can scan indeterminate, rather than rely on M-mode to split the difference.
By the way…si usted habla español, Pablo tiene un sitio Web sobre ecografía en https://ecografiaenuci.wordpress.com/